HEALTH LITERACY | May 17, 2022
Health Equity: What it Means and Why it Matters
Reading Time: 4 minutes
With more discussion than ever around healthcare’s role in achieving health equity, it’s important for healthcare professionals, healthcare organizations, and communities to have a shared understanding of the key concepts and why achieving health equity matters.
Making sense of the terminology
Here’s an overview of key health equity-related terms.
- Health equity: Essentially, health equity means that everyone has a fair and just opportunity to be as healthy as possible. Healthy People 2030 defines health equity as “the attainment of the highest level of health for all people,” noting that this requires “valuing everyone equally with focused and ongoing societal efforts to address avoidable inequalities, historical and contemporary injustices, and the elimination of health and health care disparities.” The CDC clarifies that health equity is achieved when no one is “disadvantaged from achieving this potential because of social position or other socially determined circumstances.”
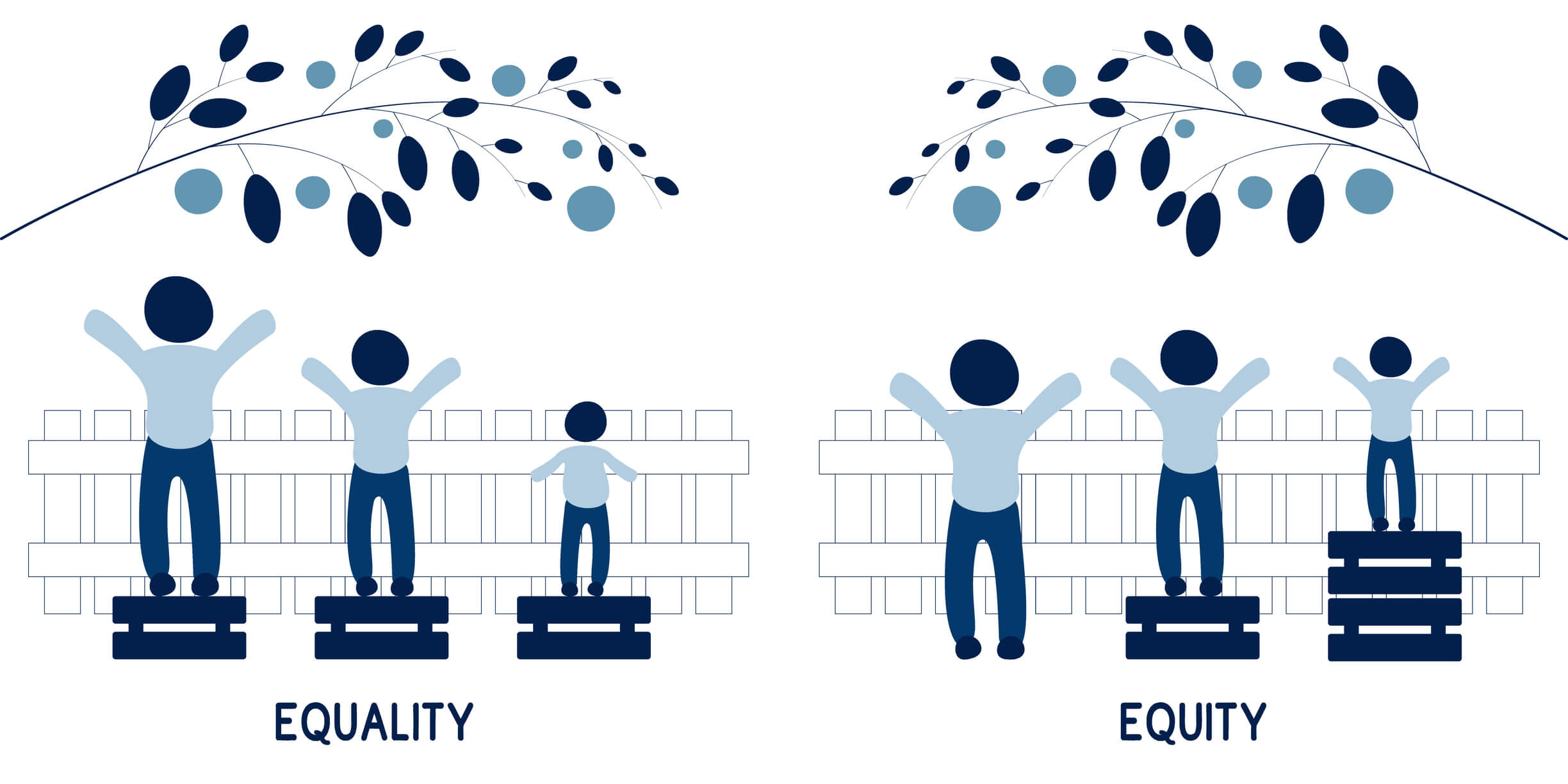
- Health equality: Health equality means that everyone is given the same opportunities, resources, access to care, and level of services to achieve optimal health. It’s important to distinguish between health equity and health equality because implementation of one of these concepts can lead to dramatically different outcomes than the other. In a system that focuses on health equality, each individual or group of people receives the exact same resources and opportunities. A health equity-driven system recognizes that each person has different circumstances and allocates the resources and care needed to reach the same level of health.
- Health disparities: Health disparities – or heath inequities – refer to differences in health outcomes between different groups of people that are systemic, avoidable, and unjust. The CDC defines the concept as “preventable differences in the burden of disease, injury, violence, or opportunities to achieve optimal health that are experienced by socially disadvantaged populations” and notes that “health inequities are reflected in differences in length of life; quality of life; rates of disease, disability, and death; severity of disease; and access to treatment.” Two stark examples of health inequities are:
-
- A life expectancy for American Indians and Alaska Natives is 4 years less than that of Americans of all other races
- A mortality rate for African American infants that is 3 times higher than non-Hispanice white infants in the U.S.
- Racism: Health disparities are rooted in racism. Defined as the structures, policies, practices, and norms that assign value and determine opportunities based on the way people look or the color of their skin, racism results in conditions that unfairly advantage some and disadvantage others, placing people of color at greater risk for poor health outcomes.
- Racial and ethnic minorities: These terms refer to populations other than Anglo-European, White, or Caucasian. The S. Department of Health and Human Services (DHHS) defines racial and ethnic minorities as American Indian and Alaska Native; Asian; Black or African American; Hispanic or Latino; and Native Hawaiian and Other Pacific Islander.
- Social Determinants of Health (SDOH): Social determinants of health refer to the non-medical factors that influence health outcomes. They are the conditions in which people are born, grow, live, work, and age that ultimately shape health. SDOH, which influence health equity in positive and negative ways, include the following factors:
-
- Socioeconomic status
- Education
- Employment
- Job security
- Food insecurity
- Access to quality healthcare
- Social support networks
- Housing, basic amenities, and the environment
- Early childhood development
- Social inclusion and non-discrimination
Understanding the impact of health inequity
While the COVID-19 pandemic shined a light on health disparities stemming from broader inequities, the issue has existed for decades. Research has shown that people of color and lower income individuals are at increased risk of being uninsured, having a shorter life expectancy, experiencing worse health status, receiving poor quality of care, and generally faring worse across a range of health measures.
Without question, health inequity affects people from disadvantaged or historically oppressed groups the most, but it also negatively impacts everyone in a society. Addressing health equity is key to improving the overall health of society and reducing healthcare costs. According to a report from the National Academies of Sciences, Engineering, and Medicine, health inequity is costly to the U.S. in terms of healthcare expenditures, national security, business viability, and economic productivity. A 2011 analysis estimated that eliminating health disparities for minorities would have reduced direct medical care expenditures by about $230 billion and indirect costs associated with illness and premature death by more than $1 trillion for the years 2003-2006. A more recent analysis concludes that the U.S. could gain $8 trillion in GDP by eliminating racial inequities.
Some of the broader implications of health inequity include:
- Elevated levels of crime and violence across communities
- Greater difficulty containing and treating infectious diseases
- Decreased productivity, employment, and tax revenue
- Larger numbers of people pushed into poverty
- More alcohol and substance misuse
- Increased stress and anxiety throughout society
- Higher cost of healthcare for everyone
Hope for the future
Given the broad implications of health inequity, reducing health disparities is a major focus for public health and government initiatives. A priority area for Healthy People 2030 is to advance health equity by eliminating health disparities and creating opportunities for people to live healthy lives.
The current administration has identified racial equity – including health equity – as a key priority, which is reflected in a series of executive orders and actions including:
- Executive Order On Advancing Racial Equity and Support for Underserved Communities Through the Federal Government
- Executive Order on Ensuring an Equitable Pandemic Response and Recovery
- The UNITE initiative
- Executive Order on Strengthening Medicaid and the Affordable Care Act
- Initiatives focused on addressing inequities in maternal health
- Presidential COVID-19 Health Equity Task Force
- Proposed Policies to Advance Health Equity
With a concerted and united effort, hopefully strides can be made in eliminating health disparities and promoting health equity.
“The route to achieving equity will not be accomplished through treating everyone equally. It will be achieved by treating everyone justly according to their circumstances.”
—Paula Dressel, Race Matters Institute
Health equity resources
- CDC’s Paving the Road to Equity initiative
- Health equity resources from the Institute for Healthcare Improvement
- The Health Equity Initiative (HEI)
- Health Equity in Healthy People 2030
- Achieving Health Equity – Robert Wood Johnson Foundation
- How to Promote Health Equity with Patient Decision Aids
ACP Decisions empowers patients and healthcare providers to engage in meaningful shared decision-making and advance care planning. Reach out today to learn how your healthcare organization can utilize our video-based patient decision aids to reduce health disparities and drive health equity – empowering all patients to engage in medical decision making.
You might also like...

How Health Literate is Your Organization?
HEALTH LITERACY | 3 MIN READ