RESEARCH | March 30, 2022
Advance Care Planning: A Tool for Healthcare Empowerment
Reading Time: 4 minutes

The onslaught of COVID-19 cases early in the pandemic derailed the process of shared decision making in healthcare by forcing in-the-moment medical decisions. The pandemic elucidated how health can deteriorate suddenly and unexpectedly, driving a call to action for individuals, families, and providers to initiate advance care planning (ACP) discussions and ensure end-of-life care wishes are documented.
ACP is an evidence-based process that identifies, documents, plans, and adjusts patients’ medical care to meet their stated goals and wishes. Ideally, ACP conversations are initiated early in every patient’s journey, advance directives and health care proxies are documented, and the healthcare team has access to this information. The reality – particularly in the face of a pandemic – is far from ideal.
New research shows that engaging patients in ACP, even during a public health emergency, elevates the opportunity for all voices to be heard when it comes to the delivery of goal-concordant and equitable healthcare.
A Clinical Trial: Promoting ACP During the Evolving COVID-19 Pandemic
In a research study recently published in JAMA Network Open, Dr. Angelo Volandes, principal investigator and Co-Founder of ACP Decisions, and an investigative team set out to determine if uptake of ACP during the pandemic would increase following implementation of video decision aids and clinician communication skills training. The team also wanted to find out how these interventions would impact ACP documentation among patients from ethnic and racial minority groups, specifically African Americans and Hispanics.
The open-cohort nonrandomized controlled trial included a large, diverse patient population aged 65 and over from twenty-two outpatient clinics in the New York metropolitan area. Documentation of a discussion about goals of care, preferences for future medical care, palliative care, hospice, or a healthcare proxy from three six-month time periods was compared: pre-COVID-19, first wave of COVID-19, and an intervention period. A large majority of the participating clinicians (84.5%) took the communication skills training.
As shown in the in the graphic below, ACP documentation was significantly greater among all groups during the intervention period, with African American patients showing the largest increase in ACP engagement.
Rates of Advance Care Planning (ACP) Documentation Overall and Among Minority Subgroups in the 3 Study Periods
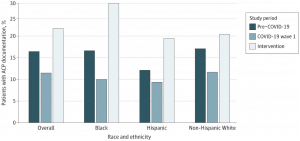
Source: Volandes AE, Zupanc SN, Paasche-Orlow MK, et al. Association of an Advance Care Planning Video and Communication Intervention With Documentation of Advance Care Planning Among Older Adults: A Nonrandomized Controlled Trial. JAMA Netw Open. 2022;5(2):e220354. doi:10.1001/jamanetworkopen.2022.0354
The Findings Have Two Significant Implications
The COVID-19 pandemic not only exposed the structural inequities to care experienced by ethnic minorities throughout the U.S., but also brought to light the immeasurable value of ACP for all patients in the face of uncertain health outcomes.
The findings from the ACP-COVID trial advocate that health systems can effectively implement ACP programs to meet the following two aims:
1.Help medical teams address urgent decisional needs during a pandemic. Healthcare systems have long had the opportunity to make sure patients’ goals of care are carried out through ACP. However, as revealed in this study, engagement has been poor with less than one in five elderly adults (aged 65 and over) having documented ACP prior to COVID-19.
The elderly population has a high risk of serious illness, hospitalization, and death from COVID-19. When hospitalized, rapid decompensation and the inability to have family nearby, leaves providers with the difficult tasks of addressing the emotional needs of family members remotely while making in-the-moment medical decisions on behalf of their critically ill patients. The ability to facilitate ACP documentation amid a public health emergency is possible, as demonstrated by the significant increase of documentation after ACP interventions during the trial.
2. Preserve the voice of ethnic and racial patient populations in the healthcare system. The disproportionate negative impact of COVID-19 on racial and ethnic minority groups is well documented. Traditionally, minorities have not embraced ACP. In a healthcare environment that is embedded with structural inequities and barriers to care, these marginalized populations need to have a documented plan to fall back on.
ACP, when carried out as a patient-centered intervention to shared decision making, is an effective tool for healthcare empowerment. The ACP-COVID trial shows that when offered ACP via an inclusive approach, both African American and Hispanic patients were much more open to having these crucial conversations. ACP offers the opportunity to elevate the voice of these individuals, giving them greater autonomy and self-determination in their care.
The study, “Association of an Advance Care Planning Video and Communication Intervention With Documentation of Advance Care Planning Among Older Adults,” was published by JAMA Open Network on February 24, 2022. You can access and read the full study here.
You may also be interested in the following articles:
- Promoting Healthcare Equity Using Patient Decision Aids
- The Vital Role of Community-Centered Care During a Pandemic
- 3 Strategies to Increase the Uptake of Advance Care Planning
- Understanding and Overcoming Vaccine Hesitancy
- The HEDIS Advance Care Planning Measure: What it is and Why it Matters
Is your healthcare organization interested in implementing or improving an ACP initiative? Contact us today to learn how we can help!
You might also like...

Recent Clinical Research in Palliative Car...
RESEARCH | 3 MIN READ

Can the COVID-19 Pandemic Improve Advance ...
RESEARCH | 2 MIN READ

Recent Clinical Research on Advance Care P...
RESEARCH | 4 MIN READ
